PARASITES
Featured on our parasite page is a selection of articles and information gathered from the World Wide Web to help you further understand the breed.
NOTE: Articles have their respected copyright owners! Most articles are collected from the top rated 100 Bengals web pages on the Internet and thus we take no responsibility, since we are not the author. We have provided credits and if you do not agree, please contact the original copyright owner. For all Bengal specific info , please check your local club.
What is coccidiosis?
Coccidiosis is a parasitic type of infection, caused by the Coccidia parasite. Coccidiosis is an intestinal tract infection caused by a one-celled organism or protozoa called coccidia. In cats and dogs, most coccidia are of the genus called Isospora. Isospora felis and Isospora rivolta are the most common species of coccidia found in cats. Coccidia are not parasitic intestinal worms. They are microscopic parasites that live within cells of the intestinal lining. Because they live in the intestinal tract and commonly cause diarrhea, they are often confused with worms. It most commonly causes watery, mucus based diarrhea in animals. If it is not treated, over time it can cause damage to the lining of a cat's intestinal tract. With appropriate and prompt treatment, the prognosis is good.
What are the clinical signs of coccidiosis?
"In kittens and debilitated adult cats, coccidiosis may cause severe, watery diarrhea, dehydration, abdominal distress, and vomiting."
Most cats that are infected with coccidia do not have diarrhea or any other clinical signs. When the eggs or oocysts are found in the stool of a cat without diarrhea, they are generally considered a transient, insignificant finding. However, in kittens and debilitated adult cats, coccidiosis may cause severe, watery diarrhea, dehydration, abdominal distress, and vomiting. In severe cases, death may occur.
Types of Coccidium that infect cats:
Isospora felis; Isospora rivolta
Sarcocystis
Toxoplamas gondi (note that this coccidial infection has zoonotic properties)
Hepatozoon – transmitted by ingestion of the 'brown dog tick
How did my cat become infected with coccidia?
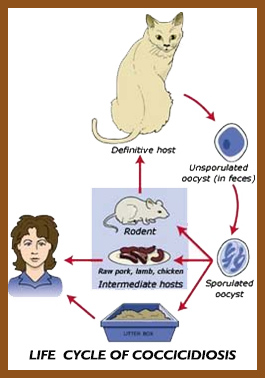
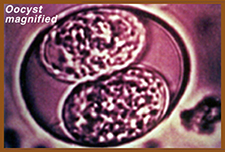
Oocysts or immature coccidia are passed in the stool of an infected cat. They lie in the environment and eventually sporulate and mature into a more developed oocyst that can re-infect the cat. Other cats, dogs, or mice may also become infected. This process can occur in as little as six hours, but it usually takes seven to ten days. If the sporulated oocysts are swallowed, they mature in the cat's intestine to complete the life cycle. If a mouse should swallow the oocysts, a cat may become infected by eating the infected mouse.
Kittens are commonly diagnosed with coccidiosis. A kitten is not born with coccidia. After birth, kittens are frequently exposed to the mother's feces. If the mother is shedding the infective cysts in her feces, her babies can ingest them during nursing. Since young kittens(less than six months of age) have no immunity to coccidia, the organisms reproduce in great numbers and may cause serious consequences.
It takes about thirteen days for illness to develop after the kitten first ingests coccidia. Consequently, kittens that become sick from a coccidial infection are at least two weeks old. Although most cases are the result of infection from the mother, this is not always the case. Any infected kitten or puppy is contagious to other kittens or puppies. In breeding facilities, animal shelters, kennels, and other areas where numerous pets may come into close proximity with one another, it is wise to isolate infected animals from those that are not
Causes
Being in an environment with other infected animals is the most common cause of this infection. It is typically spread through fecal matter, but some types may also spread through the ingestion of intermediate hosts, such as rats, mice and birds. Still, it is most commonly contracted from a parent cat to her litter due to the proximity of feces and the tendency of kittens to eat unfamiliar items and explore. The coccidiosis infection is of particular danger for kittens, since their immune systems are still underdeveloped.
How is coccidiosis diagnosed?
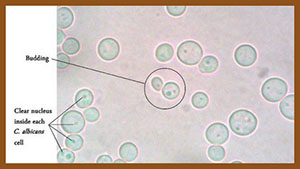
Coccidiosis is diagnosed by performing a microscopic examination of a stool sample. Since the oocysts are much smaller than the eggs of the intestinal worms, a very thorough evaluation must be performed. Infection with some of the less common coccidial parasites may be diagnosed with a special blood test.
How is coccidiosis treated?
The most common drug used to treat coccidiosis is a sulfa-class antibiotic. It is typically administered for six to fourteen days. Some formulations of this medication are pleasant-tasting and most cats will readily accept it. If the sulfa drug is not effective, other treatments are available. Additional supportive treatments may be needed if diarrhea and dehydration occur. Cats are frequently re-infected from the environment so disinfection is important. The use of diluted chlorine bleach [one cup (250 ml) of bleach mixed in one gallon (3.8 L) of water] is effective. Be sure to test clean a small area of any affected materials since bleach can damage many surfaces.
Can I get coccidiosis from my cat?
"The most common species of coccidia found in cats do not infect humans."
 The most common species of coccidia found in cats do not infect humans. Some of the less common types of coccidia are potentially infectious to humans. One of these less common species, Cryptosporidium, may be transmitted by cats or dogs to people, especially those with compromised immune systems. Cryptosporidium has also been found in public water supplies in some major cities. Another coccidial organism, Toxoplasma, is of particular concern to pregnant women because of the potential to cause birth defects in newborns. However, most human cases of Toxoplasmosis occur from eating contaminated meat as opposed to contact with a cat's feces. These two coccidial parasites pose an increased health risk for immunosuppressed humans (i.e. AIDS patients, those taking immune suppressant drugs, cancer patients, etc.). Good hygiene and proper disposal of cat feces are important in minimizing risk of transmission of all feline parasites to humans. Although there is risk of the cat transmitting these two particular parasites to humans, it does not warrant removing the cat from a home except in very rare instances, since transmission can be prevented by practicing good hygiene.
The most common species of coccidia found in cats do not infect humans. Some of the less common types of coccidia are potentially infectious to humans. One of these less common species, Cryptosporidium, may be transmitted by cats or dogs to people, especially those with compromised immune systems. Cryptosporidium has also been found in public water supplies in some major cities. Another coccidial organism, Toxoplasma, is of particular concern to pregnant women because of the potential to cause birth defects in newborns. However, most human cases of Toxoplasmosis occur from eating contaminated meat as opposed to contact with a cat's feces. These two coccidial parasites pose an increased health risk for immunosuppressed humans (i.e. AIDS patients, those taking immune suppressant drugs, cancer patients, etc.). Good hygiene and proper disposal of cat feces are important in minimizing risk of transmission of all feline parasites to humans. Although there is risk of the cat transmitting these two particular parasites to humans, it does not warrant removing the cat from a home except in very rare instances, since transmission can be prevented by practicing good hygiene.
This client information sheet is based on material written by: Ernest Ward, DVM
How is coccidiosis prevented or controlled
?
Because coccidia are spread by the feces of carrier animals, it is very important to practice strict sanitation. All fecal material should be removed. Housing needs to be such that food and water cannot become contaminated with feces. Clean water should be provided at all times. Most disinfectants do not work well against coccidia; incineration of the feces, and steam cleaning, immersion in boiling water, or a 10% ammonia solution are the best methods to kill coccidia. Coccidia can withstand freezing.
Cockroaches and flies can mechanically carry coccidia from one place to another. Mice and other animals can ingest the coccidia and when killed and eaten by a cat, for instance, can infect the cat. Therefore, insect and rodent control is very important in preventing coccidiosis.
The coccidia species of dogs and cats do not infect humans.

Baycox Dosage
The most effective treatment for Coccidiosis in kittens is to use Piglet formula Baycox liquid
(Note: Do not give to kittens younger than 4 weeks of age.)
0.1 of a cc per pound (which is one-tenth of a 1.0 cc syringe). Repeat in 10 days.
Baycox has a long "half-life" of 55 hours - that is, 55 hours after administration, 1/2 of the Baycox is still in the animal's system - so it should not be used in combination with other wormers nor repeated until at least 3 days have lapsed.
Baycox is foul-tasting, and kittens/cats will foam at the mouth. I've developed a method that makes giving Baycox fairly easy. This method also will ensure kittens do not become head shy. Most kittens like the taste of Carnation evaporated milk. Gather a small bowl of warmed canned milk, a 1.0 cc syringe to measure the Baycox, a 3.0 cc syringe for the canned milk, and a tissue. Fill the correct dosage of Baycox in the 1.0 cc syringe, and completely fill the larger syringe with canned milk. Scruff the kitten and lift (like mom would) so the back feet do not touch the counter/floor. A kitten will naturally open their mouth a bit. Place the tip of the syringe filled with Baycox between the teeth and towards the back of the tongue. Depress half the amount - slowly so the kitten doesn't aspirate. Try not to let the Baycox get on the front of the tongue. Next, while you continue to scruff, give enough canned milk closer to the front of the tongue to wash down the Baycox taste. Then give the remainder of the Baycox, and more canned milk to eliminate the Baycox taste. Let the kitten down on all fours and wipe their mouth with a tissue. If they put up any kind of a fuss about the taste, or foam at the mouth, give them more canned milk.
Once you get the hang of it, you can Baycox kittens and set them down and they will immediately run and play as if nothing negative happened. There is no head shaking, no poofed fur, and no foaming. For older kittens and mothers (who need a larger dose) give 1/3 Baycox followed by milk, another 1/3 Baycox, more milk, then the last 1/3 of the Baycox and finish with as much milk as needed. Be sure to switch syringes quickly. This method works well and it's just a matter of getting the hang of it. Try to keep the kittens/cats scruffed the entire time and get it over fast!
You can treat them if you suspect coccidia; you don't have to wait for a positive diagnosis.
This drug works best when it is used at the age of 4-6 weeks as a preventative of coccidia infection in kittens. Follow the directions carefully. Baycox does not require refrigeration.
Please note that correct Baycox (for kittens and cats) is the 5% piglet formula and not the Baycox 2.5% poultry concentrate.
An alternative to Baycox is Albon.
Helps relieve constipation in cats & dogs.
What is Lactulose Solution?
Lactulose is a type of sugar (disaccharide) that is broken down into mild acids in the end part of the intestinal tract or colon. These acids cause water to be drawn into the colon and this water helps soften the stool. Lactulose is used to treat constipation. Lactulose may also be used for purposes other than those listed in this guide.
|

|
Directions for Lactose Solution:
Lactulose Solution is a prescription medication used in dogs and cats as a laxative.
Lactulose is also used to reduce blood ammonia levels in the prevention and treatment of hepatic encephalopathy.
Lactulose Solution is not FDA approved for use in veterinary medicine; however, it is a commonly accepted practice for veterinarians to prescribe this medication for dogs and cats.
Because Lactulose is a type of sugar (disaccharide) tell your veterinarian if your pet is diabetic.
Antacids may decrease the effects of Lactulose.
What is the most important information I should know about Lactulose: Lactulose is a prescription medication that is not FDA approved for use in animals; however, it is a commonly accepted practice for veterinarians to use lactulose in dogs and cats as a laxative. Lactulose is available as a 10 Gm/15ml liquid. The usual laxative dose in dogs and cats is 1 ml per 2 pounds of body weight given every 8 hours initially, then use as needed. Notify the veterinarian if the pet develops excessive diarrhea.
What should I discuss with my veterinarian before giving lactulose to my pet: Tell your veterinarian if your pet is diabetic. Tell your veterinarian if your pet is pregnant or lactating.
Lactulose is used in cats and dogs as a laxative from your veterinarian.
Laxative
Helps
draw water into the colon to soften stool
East-to-administer liquids
Requires
veterinary prescription
For: Cats and Dogs
Benefits:
Fights a wide variety of bacterial infections•Also used to treat coccidial infections•Attacks bacterial cells, not your pet’s host cells•Albon Suspension is custard-flavored for ease of administration
How it works:
Lactulose is a disaccharide sugar composed of galactose and fructose. Unlike other sugars, its not absorbed into the blood. It passes unchanged to the large intestine. In the large intestine, lactulose is broken down by bacteria, resulting in the production of various acids. These acids draw water into the colon, softening the stool and increasing the volume, resulting in a laxative effect.
| Pet |
Weight |
Dosage |
| Dogs/Cats: |
All weights |
The usual does is 1 ml for every 2 lbs of pet's body weight every 8 hours to start, or as directed by your veterinarian, then use as needed |
Storage: Store at room temperature, away from heat and moisture.
Cautions:
It’s important for your pet to drink plenty of water. This medication should not be used in pregnant or nursing animals and should not be used in animals with liver or kidney disease.
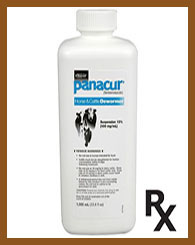
Panacur Dosage
Adults: 1.0 cc per 5 pounds, once daily, for 5 days. Repeat in 3 weeks.
Kittens: 0.25 cc per pound for 3 days. Repeat in 3 weeks.
Do not use Panacur with other wormers.
Does not require refrigeration.
Note: Metronidazole is often prescribed by veterinarians for Giardia; however, Panacur is more effective because 30% of Giardia is now immune to Metronidazole. If you do choose to use Metronidazole, the dosage: crush a 250mg tablet, mix with 10.00 cc of water, give 0.10 cc per 5 pounds (0.20 per pound).
Above information on Panacur dosage is taken from http://www.dazzledots.com/parasites.html |
GIARDIA
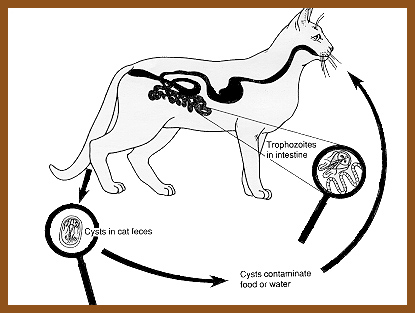
Life Cycle of Giardia in Cats
Giardia spp. are single-celled parasitic organisms (protozoa) found in the intestines of cats and many other animals. These microscopic parasites attach to the intestinal wall or swim freely in the mucous lining of the intestine (Figure1).
Approximately four per cent of pet cats in North America are expected to have Giardia. Cats less than three years of age are more often infected than older cats.
Life cycle of Giardia
Giardia occurs in two forms: a motile feeding stage (trophozoite) that lives within the intestine and a non-motile stage. The cyst develops as the parasite is swept down the intestine and before it passes in the feces. Cysts are fully developed when the enclosed protozoan divides to form two daughter organisms. The daughter trophozoites are released when the cysts are accidentally eaten. Once the parasites are released, they increase their numbers by dividing in half repeatedly.
What is Giardia?
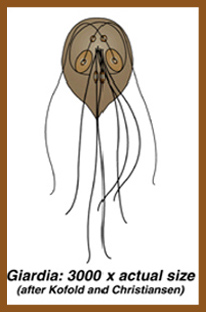 Giardiasis is an intestinal infection of man and animals cased by a protozoan parasite Giardia intestinalis (also known as Giardia lamblia). Giardia is a simple one-celled parasitic species; it is not a "worm", bacteria or virus. The parasite occurs worldwide and is a common cause of "Traveler's Diarrhea" in people. Outdoor enthusiasts who inadvertently consume contaminated water may develop "beaver fever", which is another name for giardiasis in people. Other examples of protozoan parasites that can cause enteric (intestinal) disease are Coccidia, Cryptosporidia and Toxoplasma.
Giardiasis is an intestinal infection of man and animals cased by a protozoan parasite Giardia intestinalis (also known as Giardia lamblia). Giardia is a simple one-celled parasitic species; it is not a "worm", bacteria or virus. The parasite occurs worldwide and is a common cause of "Traveler's Diarrhea" in people. Outdoor enthusiasts who inadvertently consume contaminated water may develop "beaver fever", which is another name for giardiasis in people. Other examples of protozoan parasites that can cause enteric (intestinal) disease are Coccidia, Cryptosporidia and Toxoplasma.
"Giardia is not a "worm", bacteria or virus."
The Giardia organism has two forms. A fragile, feeding form exists in the gut of infected animals. A hardy cystic form is shed in feces and can survive
several months in the environment, particularly in water and damp environments.
Giardiasis can be an important cause of diarrhea in animals and man. However, many cats are infected without developing clinical signs or the diarrhea is treated as 'non-specific'. Giardia infections in cats are undoubtedly more common than recognized or diagnosed.
The parasite has a one to two week incubation period. Most cats are asymptomatic, although they may keep passing on cysts for months or years. Clinical signs are most likely to be seen in younger animals from multi-cat households/environments.
If large numbers of trophozoites develop the cat will develop symptoms which include;
Foul smelling stools, often yellowish, foamy/frothy.
Vomiting
Weight loss
Flatulence
Abdominal distension
See more at: http://www.cat-world.com.au/giardia-in-cats
How are cats infected with Giardia?
A cat becomes infected with Giardia after swallowing the cyst stage of the parasite. Once inside the cat's intestine, the cyst goes through transformation to the trophozoite or feeding form of the organism and attaches to the intestinal wall to feed. If sufficient numbers are present, clinical signs of damage to the intestinal wall will develop. Trophozoites reproduce by dividing, and some transform into the cystic form. Eventually the cat passes cysts in its stool. These cysts are immediately able to infect another animal. Giardiasis can be transmitted by eating or sniffing the cysts from contaminated ground, or by drinking contaminated water.
"Giardiasis can be transmitted by eating or sniffing the cysts from contaminated ground, or by drinking contaminated water."
Disease is relatively rare in healthy adult cats. The likelihood of developing disease increases when large numbers of cysts are present in the environment from fecal contamination. It is more common in kittens and debilitated adult cats and is a common occurrence in densely populated groups of cats, such as in a cattery, pet store, or animal shelter. Kittens have been shown to shed more Giardia cysts in their feces than older cats.

What are the clinical signs of Giardiasis?
These microscopic parasites attach themselves to the intestinal wall and the damage causes an acute (sudden-onset) foul-smelling diarrhea. The stool may range from soft to watery, often has a greenish tinge to it, and occasionally contains blood. Infected cats tend to have excess mucus in the feces. Vomiting may occur in some cases. The signs may persist for several weeks and gradual weight loss may become apparent. The diarrhea may be intermittent. Most cats do not have a fever but may be less active. The disease is not usually life threatening but can be more serious in kittens or older cats or in cats with an immune system that has been damaged by Feline Immunodeficiency Virus (FIV) or Feline Leukemia Virus (FeLV) infections or other serious illness.
How to Know a Cat is Infected?
Clinical signs of Giardia may include pale, foul smelling feces, chronic diarrhea, weight loss or poor weight gain. Clinical signs are not always present. Infected cats may appear healthy and shed cysts.
How long does Giardia survive in the environment?
In the soil
In
cold temperatures (around 4ºC/39.2ºF), Giardia can survive for approximately 7 weeks (49 days).
At
At room temperature (around 25ºC/77ºF), Giardia can survive for approximately 1 week (7 days).
Dry vs. moist surface or environment
In a
dry, warm environment that experiences direct sunlight, Giardia can survive for only a few days[8,9].
In a
moist, cool environment, Giardia can survive for up to several weeks.
Water
In water
temperatures below 10ºC/50ºF (for example, lake water or puddle water during the winter, refrigerated water), Giardia can survive for 1–3 months.
In water
temperatures above 10ºC/50ºF (for example, river water during the fall, tap water, and puddles during the summer), Giardia can survive for less time than in colder temperatures. For example, in water above 37ºC/98.6ºF, Giardia can survive less than 4 days
What is the treatment for Giardiasis?
"Veterinary compounding pharmacies will prepare this medication in flavored formulas."
Metronidazole is the drug most commonly used to kill Giardia. This antibiotic is very bitter, so is manufactured in a coated tablet form. In order to get the correct dose for cats, the tablet must be split, thus exposing the bitter contents. To make it easier to administer the medication, veterinary compounding pharmacies will prepare this medication in flavored formulas that mask the bitterness. The medication is given orally for five to seven days.
Another antiparasitic drug, fenbendazole (Safe-Gard), is suggested as a potentially useful treatment, especially when used in conjunction with metronidazole. This combination is usually administered to cats with refractory diarrhea (diarrhea that has not responded to treatment). Supportive treatment with other drugs may be needed as supplemental therapy if dehydration or severe diarrhea is present.|
 or or 
Panacur Dosage
Adults: 1.0 cc per 5 pounds, once daily, for 5 days. Repeat in 3 weeks.
Kittens: 0.25 cc per pound for 3 days. Repeat in 3 weeks.
Do not use Panacur with other wormers.
Does not require refrigeration.
Note: Metronidazole is often prescribed by veterinarians for Giardia; however, Panacur is more effective because 30% of Giardia is now immune to Metronidazole. If you do choose to use Metronidazole, the dosage: crush a 250mg tablet, mix with 10.00 cc of water, give 0.10 cc per 5 pounds (0.20 per pound).
Above information on Panacur dosage is taken from http://www.dazzledots.com/parasites.html
Click chart for larger image


Storage: Store this product at room temperature, away from moisture and heat.
"Contaminated municipal water supplies are responsible for many outbreaks."
Further information can be found on these sites:
http://www1.agric.gov.ab.ca/$department/deptdocs.nsf/all/agdex737
http://www.cdc.gov/parasites/giardia/giardia-and-pets.html
http://www.vcahospitals.com/main/pet-health-information/article/animal-health/giardia-in-cats/119
TRITRICHOMONAS FOETUS
Tritrichomonas foetus is a microscopic single-celled flagellated protozoan parasite that has traditionally been identified as a cause of reproductive disease in cattle (infertility, abortion and endometritis).
(Try-Tricko-monas Fee-tus)
Kittens and cats living in groups have an assortment of infectious diseases to contend with: Upper Respiratory Infection, Coronavirus, and Coccidia, to name a few. Tritrichomonas foetus is yet another infectious organism yielding diarrhea in feline patients, usually with a history of group lifestyle. This organism was previously thought to infect only cattle, where it causes miscarriage and fertility problems, but recently (in 2003) T. foetus has emerged as an infectious agent for cats. Information and recommendations regarding this organism have changed in the last several years and we attempt to provide the most up to date summary of what is known and recommended for prevention and treatment of this infection.
What is Tritrichomonas Foetus Anyway?
The short answer is that this is a single-celled organism. The longer version is that this is a flagellate, a single-celled organism possessing lash-like structures called flagella on its body, which wave around allowing the organism to move. T. foetus is commonly mistaken for Giardia, another parasitic flagellate; they both use flagella to move around and both have pear shaped bodies.
How do Cats get Infected?
T. foetus organisms are shed in the feces of an infected cat. Most commonly, transmission occurs when cats share a litter box as the organism can live up to 3 days in fecal material. Any time a cat steps in the feces of an infected cat, organisms can be transferred to the paws and later licked up during grooming.
What does it do to a Cat?
T. foetus colonizes the lower intestine of the cat causing the mucous and sometimes bloody diarrhea that characterizes Colitis. If the colon is biopsied, inflammatory cell infiltration typical of Inflammatory Bowel Disease will be seen. Infected cats do not always have diarrhea; many cats, especially older ones, have no symptoms at all but are still contagious to other cats.
Because colitis can have so many causes, it is important to keep this possible cause in mind. Chronic colitis may or may not respond to symptomatic treatment and if a specific underlying cause can be identified and treated, a long-term difficult problem can be potentially resolved permanently. Many colitis remedies will lead to temporary improvement for a Tritrichomonas-infected cat but the symptoms generally come right back after treatment ceases.
Making the Diagnosis
There are presently four testing methods that can be used to identify Tritrichomonas foetus in a fecal sample. It should be noted that a proper fecal sample for testing must be freshly voided (i.e. immediately retrieved from the anus with no cat litter contamination), obtained with a deeply inserted fecal loop, or flushed from the colon with a syringe. Bringing a sample from home will not be adequate. If the cat has been on antibiotics, this will interfere with testing; the cat should be off antibiotics for at least a couple of days.
Direct Smear
Some fecal matter is swabbed onto a microscope slide, mixed with a gentle saline solution, and examined for flagellate organisms. The feces must be immediately fresh from the rectum. The wetter and more mucous the sample is, the better. Usually several slides must be examined as the organism is elusive. Standard fecal tests for parasites will not pick up this organism. Refrigeration of the sample will kill the organism and make it impossible to detect. Further, if the patient is on antibiotics the number of organisms available to detect will be greatly reduced even though most antibiotics cannot cure the infection.
While this is a relatively easy test to perform, it only has about a 14% chance of detecting a natural T. foetus infection. A more sensitive test is generally preferred.
Culture (also called the Pouch Test)
A specific culture bag can be used to grow T. foetus in numbers large enough for detection. The feces used must be freshly obtained from the rectum, inoculated into the pouch, and the pouch is kept in a vertical position for 12 days at room temperature. The pouch is periodically examined under the microscope for the presence of organisms.
This is the test method of choice in most cases as it is easy to perform, reasonably priced and generally accurate.
PCR Testing (Polymerase Chain Reaction Testing)
PCR testing is a DNA test for the presence of T. foetus. A larger fecal sample is needed and the test must be done at a reference lab. It is generally reserved for patients where the pouch test has been negative but the index of suspicion is still high.
PCR testing is the most sensitive of all the test methods but is also fairly expensive. Specialized equipment is needed and only a few laboratories are qualified to run samples.
Biopsy
A routine colon biopsy is unlikely to find this parasite; specific stains on the tissue (immunohistochemistry) must be requested and at least six tissue samples must be examined. This is the most invasive form of testing and would not be done right off the bat but if the patient is going to have a biopsy for chronic colitis anyway, it might be a good idea to have the pathologist look for T. foetus.
A negative test never rules out Tritrichomonas infection,
no matter which test is performed.
 OWNERS GUIDE TO DIAGNOSIS AND TREAT TRITRICHOMONAS FOETUS OWNERS GUIDE TO DIAGNOSIS AND TREAT TRITRICHOMONAS FOETUS
 Diarrhea-Tritrichomona Diarrhea-Tritrichomona
TREATMENT
In the past, several different antibiotics have been reported to be effective but it turns out that this is probably an overestimate since 88% of cats will resolve their diarrhea spontaneously within 2 years. They will still be infected, or at least 57% of them will be, but they will have normal stool and they may relapse with stress. One treatment option is to simply wait for resolution if the household does not have a large number of cats and the diarrhea is not excessive. The only drug that is felt to be reliable against T. foetus is ronidazole, and its use is far from straight-forward. Here is what to know: Ronidazole must beCompounding to get a dose in a suitable size for cats. Ronidazole is not licensed for use in cats; it is a poultry antibiotic. It also tastes really bad and should be provided in capsules rather than as an oral liquid to avoid the taste. People must wear gloves when handling ronidazole. The most common side effect in cats is neurotoxicity, which means it is not appropriate to use ronidazole as a trial to see if a cat with colitis improves on it. Ronidazole should be used only in confirmed Tritrichomonas patients. Neurotoxicity manifests as loss of appetite, incoordination, and possibly seizures. Some experts recommend engaging the cat in play on a daily basis to assess muscular coordination and agility.
Cats being treated should be isolated from other cats in the home to prevent reinfection. It is not possible to fully confirm that an infection has been eradicated as a negative PCR test does not rule out infection. Experts recommend a PCR test in 1 to 2 weeks after treatment and again 20 weeks after treatment as the closest we can come to confirming eradication.
Ronidazole is usually given once daily for 2 weeks. The diarrhea should be resolved by the end of this course.
This information was gathered http://www.veterinarypartner.com/Content.plx?A=2830
IMODIUM TO STOP SERVERE DIARRHEA
|
Use Imodium To Stop Severe Diarrhea
Loperamide Hydrochloride Tablets USP 2 mg
High end dose: dissolve one table (2 mg) into 27.5 cc water. Give 0.1 cc per pound.
Low end dose: dissolve one table (2 mg) into 55.0 cc water. Give 0.1 cc per pound.
Give the above dose once or twice. |
CREDITS:
http://www.1800petmeds.com/Lactulose+Solution-prod10665.htm
http://www.vcahospitals.com/main/pet-health-information/article/animal-health/coccidiosis-in-cats/73
http://www.1800petmeds.com/Albon+Suspension-prod10336.html
http://www.dazzledots.com/parasites.html
Note: Kaopectate is not safe for use with cats.
Disclaimer: I am not a veterinarian, and this information is not intended to replace veterinary diagnosis or treatment. If you have a kitten who is ill, please take it to your vet for treatment IMMEDIATELY.
BACK TO TOP
|
 |
©Copyright 2015 - 2019 RIV Media All Rights Reserved
|
|
|
|